Research Program
Our research program for 2022 to 2025 has a pronounced focus on osteoarthritis (OA). It is structured in two comprehensive Program Lines:
- Pathophysiology of the Joint
- Clinical Research,
and an additional Service Line.
The Program Line Pathophysiology of the Joint covers basic and translational research. It aims
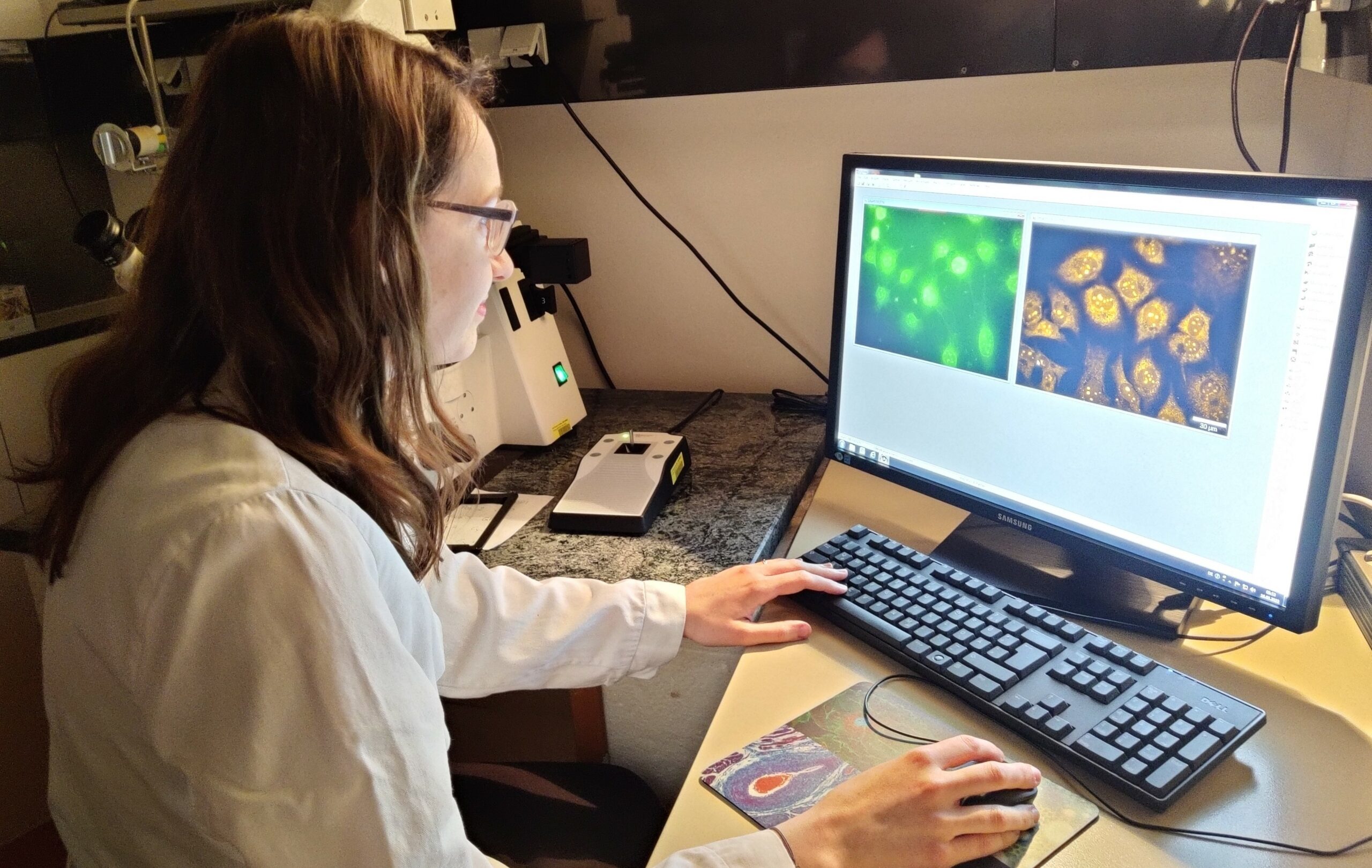
- at further elucidating the cellular and molecular mechanisms of OA using state-of-the-art methodology,
- on individualising treatment through better prediction based on biomarkers including epigenetics, and
- finding potential novel therapeutic targets.
Exploring the molecular pathways in chondrocytes and synovial fibroblasts is a prerequisite for understanding disease mechanisms in OA and other joint diseases and is especially important when searching for novel targets for therapy.
The Program Line Clinical Research focuses on
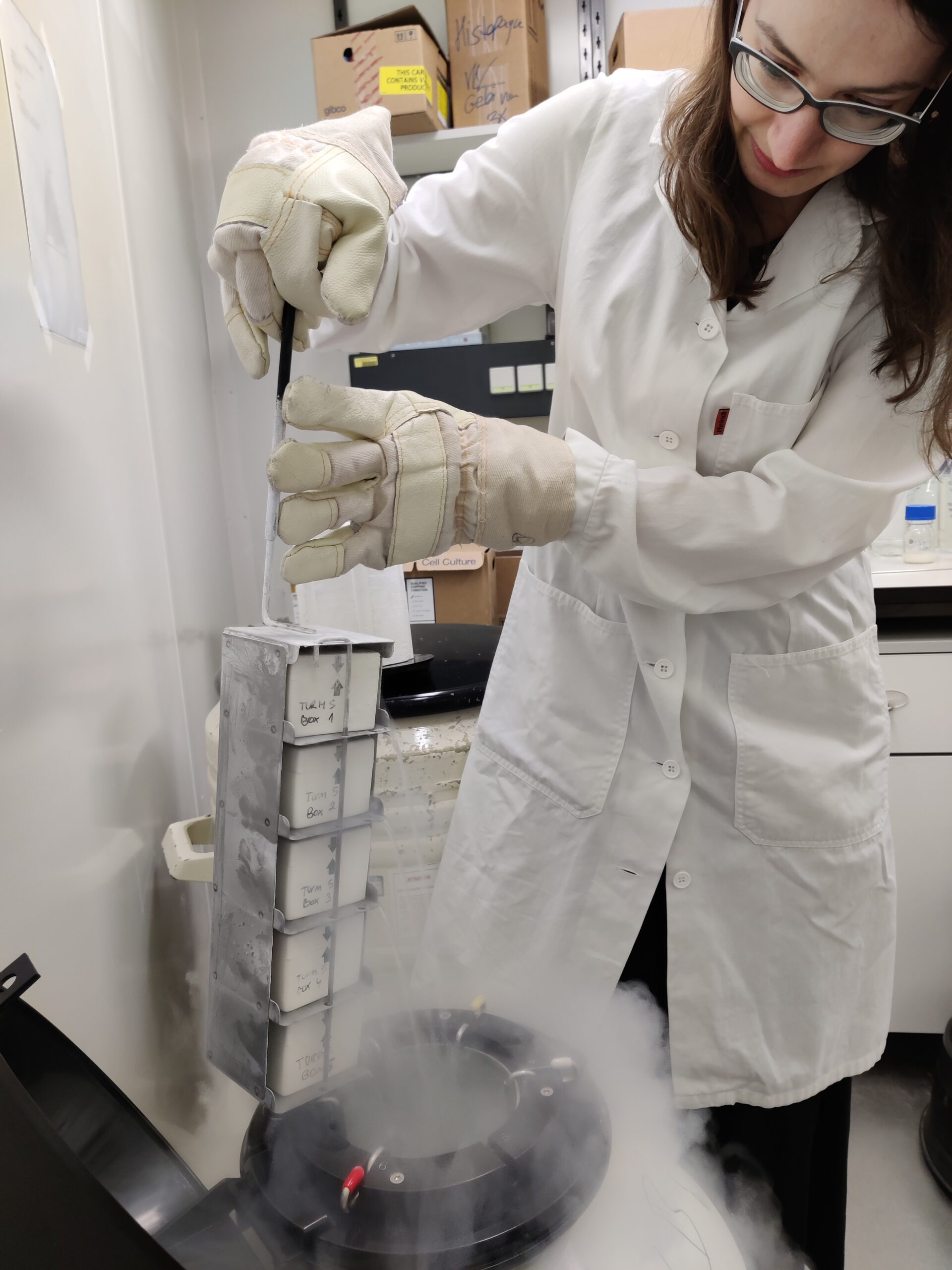
- building up a large cohort and bio-material bank of people with OA including clinical and laboratory parameters, biomarkers and bio-samples, images, risk factors, oral health and patient-reported outcomes, as a common good and for common use within the LBIAR;
- individualising treatment through better prediction based on clinical (phenotypes) as well as psycho-socio makers, especially considering return to work rates, activities in daily life and participation; and
- advancing algorithms for the analysis of imaging data of the osteoarthritic joint by magnetic resonance imaging and ultrasound.
The Service Line covers studies which are specifically commissioned by a partner or an external third party.
b. Exploring the molecular pathways in chondrocytes and synovial fibroblasts is a prerequisite for understanding disease mechanisms in OA and other joint diseases.
c. Our Clinical Research focuses on advancing algorithms for the analysis of imaging data of the osteoarthritic joint by magnetic resonance imaging and ultrasound
d. Our institute is also building up a large cohort and bio-material bank of people with OA including clinical and laboratory parameters, biomarkers and bio-samples, images, risk factors, oral health and patient-reported outcomes.